
Robert C. Garrett is Co-CEO of Hackensack Meridian Health, which has four hospitals ranked among the top 10 in New Jersey according to U.S.News & World Report – including No. 1 ranked Hackensack University Medical Center – more than any other network in the state. Robert focused on aggressive expansion of the Hackensack University Network before its merger with Meridian Health. As Co-CEO, Robert concentrates on innovation and leading partnerships, including launching New Jersey’s first private medical school with Seton Hall University and a historic partnership with Memorial Sloan Kettering Cancer Center.
 John K. Lloyd is Co-CEO of Hackensack Meridian Health, one of the largest, most comprehensive health networks in New Jersey, which includes 13 hospitals, 28,000 team members, more than 6,000 physicians and over 140 patient care locations across the state. John has focused much of his career on developing a full continuum of care – long before national health care reform mandated such changes. As Co-CEO, John oversees all non-acute care hospital businesses, including population health and the foundations. John’s expertise and vision have helped the network meet and exceed the challenges of health care reform.
John K. Lloyd is Co-CEO of Hackensack Meridian Health, one of the largest, most comprehensive health networks in New Jersey, which includes 13 hospitals, 28,000 team members, more than 6,000 physicians and over 140 patient care locations across the state. John has focused much of his career on developing a full continuum of care – long before national health care reform mandated such changes. As Co-CEO, John oversees all non-acute care hospital businesses, including population health and the foundations. John’s expertise and vision have helped the network meet and exceed the challenges of health care reform.

Patrick R. Young is president of Population Health for Hackensack Meridian Health, where he leads the PopulationHealth division and is responsible for accelerating the development of strategic priorities related to health care reform; population health management; Meridian’s Medicare Shared Savings Accountable Care Organization; Hackensack Meridian Health Partners, Hackensack Meridian Health’s clinically integrated network; health insurance partnerships; as well as overseeing Managed Care.
Key Takeaways
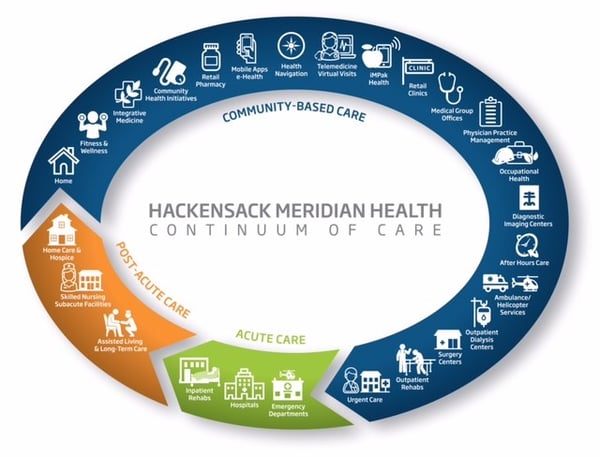
- In a merged system comprised of multiple entities, a continuum of care model – which focuses on coordination and collaboration between healthcare providers – is essential to enhance the patient experience and deliver value.
- Data integration and analytics – whereby provider, payer, and pharmaceutical data come together in one location – is a key ingredient for predictive modeling that allows providers to proactively manage the health and wellness of their patients to enhance outcomes.
- As a health system, it is critical to pay attention to the social determinants of health because it allows for a more holistic approach to patient care rather than just focusing on the delivery of clinical care.
TLD Group: How do you define your health ecosystem?
Lloyd: I was recruited as president of Jersey Shore Medical Center in 1982 as a traditional hospital administrator. However, I knew that we would need to offer ambulatory services to enable us to increase access for patients. With that focus, we began to develop our continuum of care. I led the merger of several hospitals in Ocean and Monmouth Counties to create Meridian Health. As our system grew, our goal was to ensure that there was a Meridian service within 15-20 minutes of every resident in the two-county area. We merged with Hackensack University Health Network to increase our reach into northern New Jersey. Through this merger, we now have a massive continuum of care (see Figure below). The CEO of the Hackensack network, Bob Garrett, has been a friend for over 25 years. For a defined period of time, Bob and I will serve as co-CEO’s, which defies all the leadership books.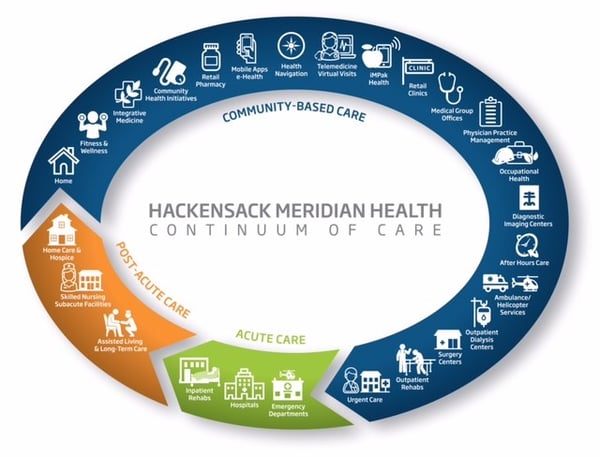
TLD Group: How did you align stakeholders to enable a successful continuum of care model?
Garrett: We had hundreds of people involved in building this process from the bottom up, rather than from the top-down. We redesigned the structure and the process by going out to the care coordinators, the nurses, the physicians, etc. and asked, “How can we make this better?” However, it is our responsibility as leaders to show the benefits of this process and ensure it is fully embraced. It’s essential that we convey how our signature quality as a network – focusing on the full continuum of care – results in better care and cost savings not just for Hackensack Meridian Health, but for the nation’s health system. Let me provide a quick example. Health care expenditures consume one-sixth of our entire economy – up from 5% in 1960. Treatment in hospitals consumes about one-third of these expenditures. That’s why we are expanding urgent care centers and other outpatient options – on our own and with partners – so that our patients get high quality care at the right place and time and for the right cost. This is our north star, especially when costs will only increase with the aging of the nation’s 76 million baby boomers. Diseases such as Alzheimer’s and other forms of dementia are costing our country $259 billion this year. By 2050, the costs could exceed $1 trillion if we don’t slow the arc of health care spending.
TLD Group: How do you coordinate care across such a vast care continuum?
Young: When it comes to care coordination, we have care managers on our population health team, in our patient centered medical homes, embedded in select practices in our clinically integrated network, at the acute facilities, and at the post-acute centers. In earlier times, they were all operating in silos despite working in the same organization. Over the last two years, we’ve engaged a healthcare strategy firm, GE Healthcare Camden Group, which helped us facilitate and coordinate the entire continuum of care so that we operate as one cohesive organization. We began consolidating our care coordinators under population health to streamline the process between physicians, case management, nurses, social workers, etc. – all working together across our entire system to enhance the patient experience and deliver care more efficiently.
Much of this progress is tied to what’s known as value-based care, a big step from traditional fee-for-service medicine. The core change is that doctors and hospitals are paid to keep patients healthy, through Accountable Care Organizations (ACOs).
Under the traditional fee-for-service model, hospitals and physicians get paid for every treatment or hospitalization, so the cost of care – especially for patients with chronic disease – is typically an expensive revolving door with little monitoring of cost or outcome. In contrast, ACOs closely track patients and make sure they get help before a problem becomes serious – and expensive.
Additionally, Dr. Andrew Pecora, our Chief Innovation Officer, is working on the clinical care transformation to mitigate the variance in care from a clinical standpoint. Physicians practice differently, but if you can bring some consistency through scientific methodologies and combine that with care coordination, you can change the whole paradigm.
TLD Group: What role does collaboration play in enhancing the health of communities you serve?
Garrett: We have several innovative, collaborative initiatives underway that go to the heart of our mission. Most notably, we have a 10-year strategic partnership with Memorial Sloan Kettering Cancer Center (MSK) to expand and enhance cancer care in New Jersey with more outpatient options, access to 800 clinical trials and an exceptional, uniform treatment protocol. We believe this is a great opportunity for two national leading cancer centers to join forces. With this strategic partnership, we look forward to offering patients the most innovative treatment close to home.
This summer, Hackensack Meridian Health, in partnership with the New Jersey Innovation Institute, an affiliate of the state’s largest technology university, launched the state’s first incubator to improve health care. The network contributed $25 million, a new revenue stream to help companies develop trailblazing products and services. Already 10 companies have pitched ideas – including a device to lower risk in laparoscopic surgery and a wearable monitor to better track patients’ vitals. Four have been selected to reach the finals where we begin the concept of commercializing the idea.
Additionally, the medical school we are launching with Seton Hall University will not only transform medical education but keep more doctors in New Jersey where they are needed.
TLD Group: What is the biggest challenge to enhancing the health of the communities you serve?
Young: We have a very fragmented health care system today in our country. Our organization has made great progress in coordinating care, but there are still a significant number of services provided by independent agencies and we don’t have systems that communicate well with them. When I came to this organization there was a lot of data. But the question is, how do we make that data useful and how do we get it to physicians in a timely and appropriate manner? We decided to develop our own data warehouse, so we could control the data. This way, we gather and store the clinical data that we collect in real time through Epic, as well as claims data from payers, pharmacy data, background information, etc. All of these different pieces of information come together in one location to give us a complete view of our patients. We’re utilizing that information to work with our care managers and have even begun some predictive modeling. Based on the information we have, we may be able to identify potential issues for patients. My data analytics team – clinical pharmacists, population health scientists, data analysts, etc. – provide our physicians and care managers with this information so they can reach out to patients proactively. This is transformational work – and it’s leading to great outcomes. For example, we had a congestive heart failure patient who tracked and sent her daily vital signs through an iPad provided by our care managers. Her assigned care manager was able to track this patient’s progress and proactively intervene if any readings were cause for concern. This novel approach reduced this patient’s hospital admissions and enabled her to lead a more active life. The current challenge is effectively organizing everyone and facilitating a useful means of the data we have.
TLD Group: What is the significance of addressing the social determinants of health?
Lloyd: The social aspects of our patients’ lives are critically important. Let’s say your hospital readmission rates are higher than average, and you want to determine why people are being readmitted. It may be as simple as the patient not eating well when he is discharged. But why isn’t the patient eating well? Perhaps there’s no option to eat three good meals a day. As a health care provider, we don’t get paid to provide meals for patients. But if we’re getting paid for the outcomes, and we don’t want that person to be readmitted, we need to begin to think differently about where our role in care delivery really ends. As a health system, we need to be paying attention to the social determinants because it allows us to approach patient care from a holistic point of view rather than just focusing on clinical care.
View our other HELM Q&A Interviews:


 John K. Lloyd
John K. Lloyd



 Andrew Baskin, MD, is Aetna’s Vice President, National MedicalDirector for Quality and Clinical Policy and served as the Interim Chief Medical Officer (in 2014). He works on initiatives to measure and improve quality of care, the provision of evidence based care, quality measurement implementation and public reporting, health plan accreditation, and the establishment of performance based networks. Additionally, Andy partners with others to help establish programs which create incentives for more effective and efficient care, influence and assure compliance with healthcare reform regulations, develop products to improve affordability and quality of care, and promote payment reform.
Andrew Baskin, MD, is Aetna’s Vice President, National MedicalDirector for Quality and Clinical Policy and served as the Interim Chief Medical Officer (in 2014). He works on initiatives to measure and improve quality of care, the provision of evidence based care, quality measurement implementation and public reporting, health plan accreditation, and the establishment of performance based networks. Additionally, Andy partners with others to help establish programs which create incentives for more effective and efficient care, influence and assure compliance with healthcare reform regulations, develop products to improve affordability and quality of care, and promote payment reform. Mohamed Diab, MD, Vice President of Provider Transformation leads population health management at Aetna. His focus is on providers as they transform their care delivery to achieve the “Triple Aim” by improving quality of care and reducing unnecessary cost. Mohamed has more than 25 years of experience as a provider as well as an executive in the payer and consulting industries. He has a background in medical management, pharmacy benefit management, clinical informatics and cost management programs.
Mohamed Diab, MD, Vice President of Provider Transformation leads population health management at Aetna. His focus is on providers as they transform their care delivery to achieve the “Triple Aim” by improving quality of care and reducing unnecessary cost. Mohamed has more than 25 years of experience as a provider as well as an executive in the payer and consulting industries. He has a background in medical management, pharmacy benefit management, clinical informatics and cost management programs.







 Robert C. Garrett is Co-CEO of Hackensack Meridian Health, which has four hospitals ranked among the top 10 in New Jersey according to U.S. News & World Report – including No. 1 ranked Hackensack University Medical Center - more than any other network in the state. Robert focused on aggressive expansion of the Hackensack University Network before its merger with Meridian Health. As Co-CEO, Robert concentrates on innovation and leading partnerships, including launching New Jersey’s first private medical school with Seton Hall University and a historic partnership with Memorial Sloan Kettering Cancer Center.
Robert C. Garrett is Co-CEO of Hackensack Meridian Health, which has four hospitals ranked among the top 10 in New Jersey according to U.S. News & World Report – including No. 1 ranked Hackensack University Medical Center - more than any other network in the state. Robert focused on aggressive expansion of the Hackensack University Network before its merger with Meridian Health. As Co-CEO, Robert concentrates on innovation and leading partnerships, including launching New Jersey’s first private medical school with Seton Hall University and a historic partnership with Memorial Sloan Kettering Cancer Center. John K. Lloyd is Co-CEO of Hackensack Meridian Health, one of the largest, most comprehensive health networks in New Jersey, which includes 13 hospitals, 28,000 team members, more than 6,000 physicians and over 140 patient care locations across the state. John has focused much of his career on developing a full continuum of care – long before national health care reform mandated such changes. As Co-CEO, John oversees all non-acute care hospital businesses, including population health and the foundations. John’s expertise and vision have helped the network meet and exceed the challenges of health care reform.
John K. Lloyd is Co-CEO of Hackensack Meridian Health, one of the largest, most comprehensive health networks in New Jersey, which includes 13 hospitals, 28,000 team members, more than 6,000 physicians and over 140 patient care locations across the state. John has focused much of his career on developing a full continuum of care – long before national health care reform mandated such changes. As Co-CEO, John oversees all non-acute care hospital businesses, including population health and the foundations. John’s expertise and vision have helped the network meet and exceed the challenges of health care reform. Patrick R. Young is president of Population Health for Hackensack Meridian Health, where he leads the Population Health division and is responsible for accelerating the development of strategic priorities related to health care reform; population health management; Meridian’s Medicare Shared Savings Accountable Care Organization; Hackensack Meridian Health Partners, Hackensack Meridian Health’s clinically integrated network; health insurance partnerships; as well as overseeing Managed Care.
Patrick R. Young is president of Population Health for Hackensack Meridian Health, where he leads the Population Health division and is responsible for accelerating the development of strategic priorities related to health care reform; population health management; Meridian’s Medicare Shared Savings Accountable Care Organization; Hackensack Meridian Health Partners, Hackensack Meridian Health’s clinically integrated network; health insurance partnerships; as well as overseeing Managed Care.































































